Investigating Daily Practices of Self-care to Inform the Design of Supportive Health Technologies for Living and Ageing Well with HIV
Digital Health


Collaborators Northumbria University, UCL, University of Edinburgh, City University of London, University of Bristol, NHS, Terrence Higgins Trust, Public Health England, National Aids Trust, Microsoft Research, YOTI, INTEROPen, UK-CAB
Abstract
We report on a Diary Study investigating daily practices of Self-care by seven UK adults living with HIV, to understand their routines, experiences, needs and concerns, informing Self-care technology design to support living well.
Method
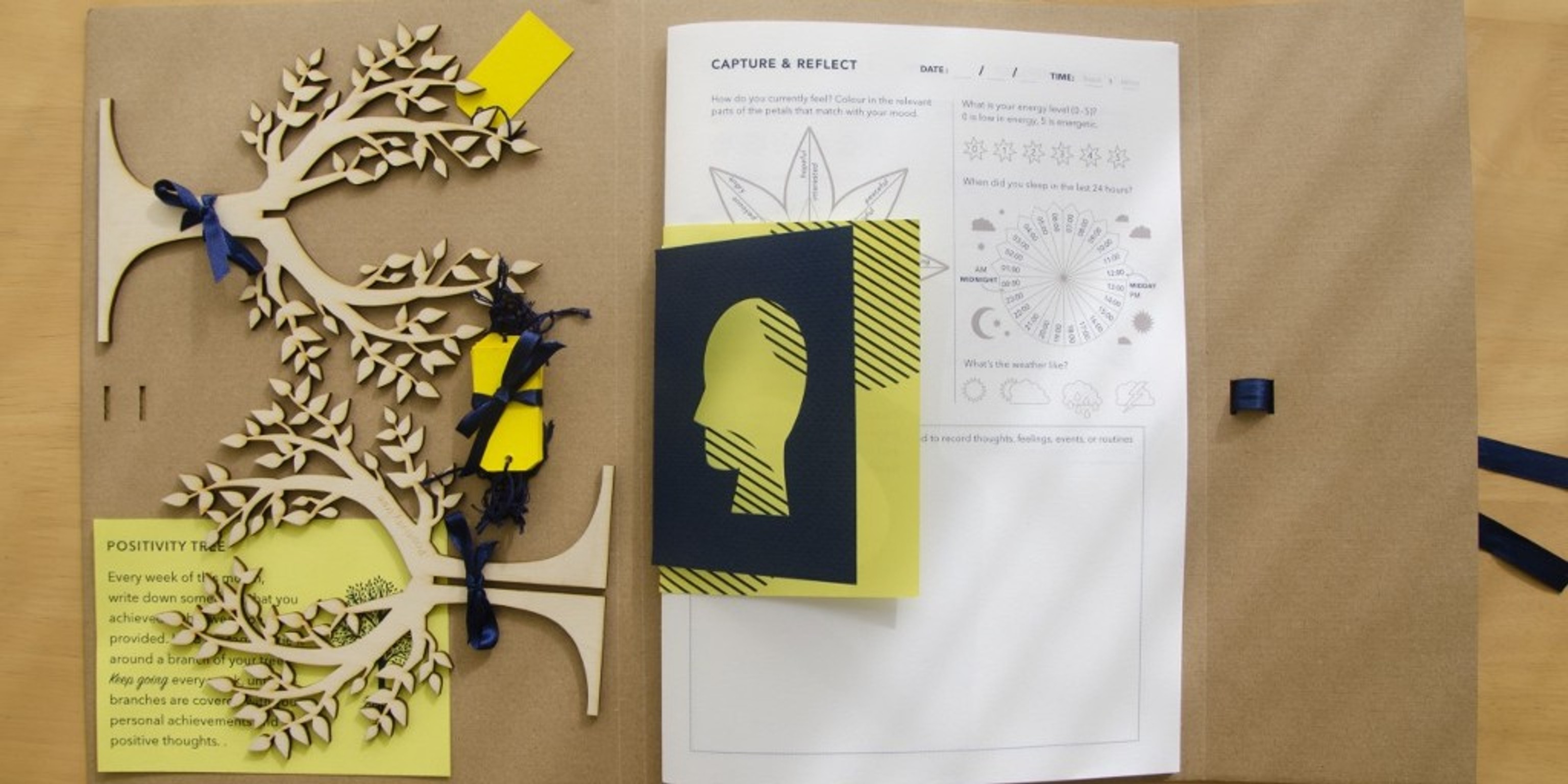
We designed a bespoke paper diary, which was deployed with participants as a vehicle for critical inquiry, to evidence the psychosocial complexities for practicing Self-care. The Diary deployment was supported by interviews, which enabled us to discuss potential barriers to technology use related to trust, privacy, and representation, gaining new significance during the COVID-19 pandemic.
Takeaways
Our evaluation of using a Self-care Diary as Design Probe responds to calls to study Self-care practices so that future digital health tools are better grounded in lived experiences of managing multi-morbidity.
We report on a Diary Study investigating daily practices of Self-care by seven UK adults living with Human Immunodeficiency Virus (HIV), to understand their routines, experiences, needs and concerns, informing Self-care technology design to support living well.
We advance a developing HCI literature evidencing how digital tools for self-managing health do not meet the complex needs of those living with long-term conditions, especially those from marginalised communities.
Our evaluation of using a Self-care Diary as Design Probe responds to calls to study Self-care practices so that future digital health tools are better grounded in lived experiences of managing multi-morbidity. We contribute to HCI discourses including Personal Health Informatics, Lived Informatics and Reflection by illuminating psychosocial challenges for practicing and self-reporting on Self-care.
Design implications
We offer design implications from a Critical Digital Health perspective, addressing barriers to technology use related to trust, privacy, and representation, gaining new significance during the COVID-19 pandemic.
We offer to HCI researchers a Critical Health Studies Perspective in a post-pandemic context on considerations for designing Self-care technologies for adult populations living with and managing multiple Long-Term Conditions (LTCs), focusing on the complex socio-medical context of living with HIV in the UK.
Our empirical study findings have grounded discussion on how the mundane practices of Self-care may contribute to the coordination of Whole-person Care and may be empowering for Patient-involved Care.
Our critical approach has guided us through an analysis of the challenges and barriers to practicing Self-care and the use of non-digital tools with digital tools for self-reporting on these practices and experiences.
We find self-reporting practices valuable to people with HIV for fostering bodily awareness and self-efficacy, for supporting the non-trivial task of balancing emotional wellbeing and sustaining long-term care management and QoL.
Material for designing self-care technologies
Our insights provide ‘material for designing self-care technologies’ that better support the mundane and psychosocial dimensions of living and ageing with LTCs such as HIV.
We encourage interaction designers to consider the appropriateness of non-digital elements in Self-care service structures that accommodate tangible or hybrid interactions with digital and low-tech elements.
In the context of LTC management, our findings suggest design directions for emotional support that facilitates productive work with negative emotions. Designers must address how people can be supported in building a routine over time or picking up a routine when broken.
We provide insight on the service users perspectives, highlighting a design space to better support them in organising self-captured information ahead of the consultation – not necessarily for presenting that information but, rather, to increase confidence in their communication about how they are involved in their treatment and care.
With a perceived pressure or government-led requirement to use remote or online forms of communication, those who may feel particularly vulnerable, experiencing low mood, Anxiety and other barriers to Self-care (e.g. those who are newly diagnosed or older adults with HIV) may be disadvantaged or compromised because they may not be ready to share information about their wellbeing, their life, and their Selfcare practices online. Tools for sharing and communication must be designed with Trust features as a core requirement.