Using technology to self manage long term conditions
In this blog post on the relationship between an issue of importance in HCI and an issue of importance in digital civics I would like to consider the role of technology in the self management of long term conditions (LTCs). I am particularly interested in how technology is used by people with invisible illnesses or disabilities to self-manage their condition. In my post I will be drawing upon academic papers, web resources and previous blog posts (my own and those of my fellow course members).
I will first briefly outline why long term conditions/invisible illness are an important social issue. I will then discuss two areas within HCI that are particularly relevant to this – personal informatics and online communities – and how people with LTCs are using these technologies. I will follow this by considering how the phenomena of using these technologies to self manage LTCs relates to digital civics; specifically, the implications for new models of citizen-led services and the concept of the ‘digital citizen’ in health and social care.
I will conclude by asking what future research could be done in this area. Throughout this post I will add my personal opinion on where I believe technology can be helpful to self management and where I feel we should exercise caution.
Long term conditions, self management and ‘invisible illness’
The Western world is experiencing a dramatic increase in the proportion of people living with long term health conditions; those conditions for which there is no cure, for example, arthritis or diabetes. One in five people in the UK lives with a LTC and increasing numbers of people are living with multiple LTCs [2]. On average, people with LTCs spend just three hours a year with their healthcare team; the rest of the time they are self managing their condition [39].
In the context of health and social care, self management encompasses any tool, technique or treatment that a person uses to manage their condition. Peer support groups, relaxation techniques, self monitoring of various symptoms, following diet and exercise regimes are all examples of self management. There can be particular problems of misunderstanding and stigma when people have a health problem which is not obvious to others, sometimes known as ‘invisible illness’ [18].

Many people with LTCs are already using technology to help them self manage. Mankoff et al suggest that this type of active role is more likely when a condition is chronic [25]. Increasingly, this is of interest to policy makers, for example NHS Education for Scotland recently produced this report on the use of social networking in the self management of long term conditions [12].
Personal informatics
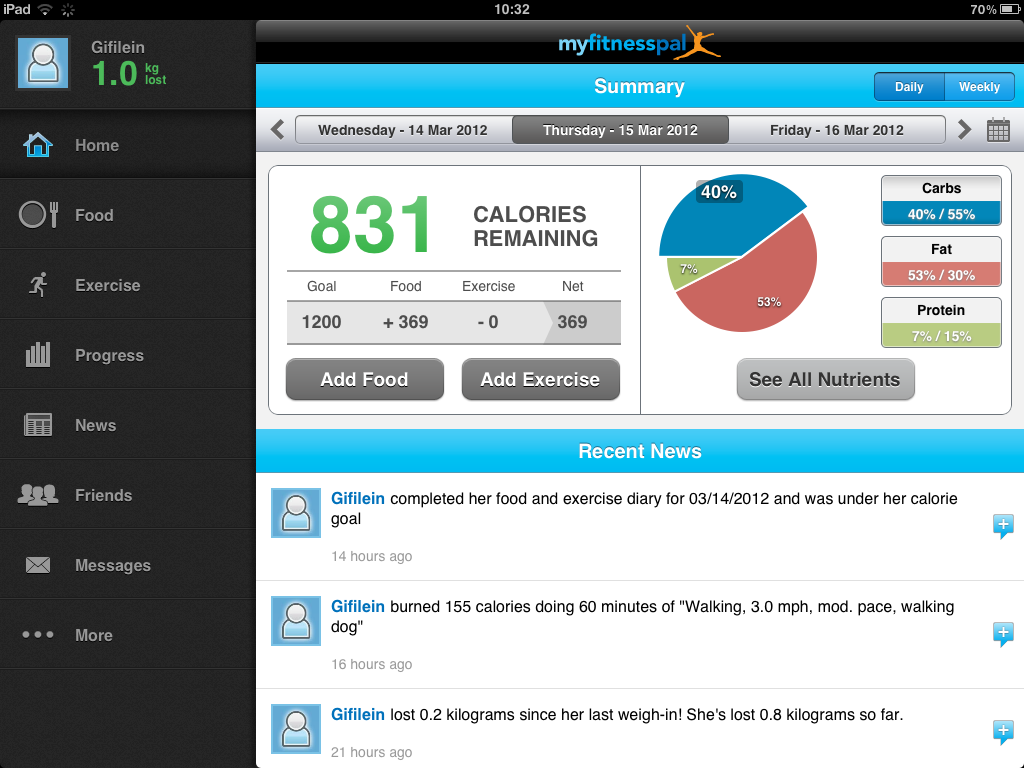
With the growth of ubiquitous computing, wearables and the expansion of computing beyond the workplace and into every aspect of our lives (also known as ‘the third wave of HCI’ [4]) there has been increasing interest within HCI in personal informatics and tracking. Personal informatics systems (PIS) and tools are frequently framed as means by which we can monitor our health and gain information that we can use to change our behaviour and improve our wellbeing. A common example of a personal informatics tool is the Fitbit – an activity tracker which can be worn round the wrist and measures data such as number of steps walked, quality of sleep and other personal metrics. Another example would be the smartphone app My Fitness Pal where users manually enter in their food consumption and log their exercise for the day.
In the opening to their seminal paper on a stage-based model of PIS Li, Dey & Forlizzi [17] assert that ‘people strive to attain self-knowledge’. In a previous blog post I was sceptical of the very rational and cognitive stance adopted by their paper. During our sessions on personal informatics I found I was much more sympathetic to the idea of ‘lived informatics’ from Rooksby et al [34], as reviewed by Nataly in her blog post. As someone who is interested in the sociology of the body I was already predisposed to thinking about the ways in which the data from this type of ‘self’-tracking is socially embedded and produced. I therefore drew heavily on Lupton’s work when thinking about this topic [19] and the paper reviewed by Dan for his blog post was of particular interest [22].
However, I also acknowledged that I have personally used self-tracking tools to manage multiple LTCs. This led me to explore the increasing HCI and health literature on how people with LTCs are making use of personal informatics to self manage their body and/or illness.
Personal tracking has become part of a whole movement: The Quantified Self . In their blog posts Eujin and Janis wrote about some of the complications around collecting personal data in this way such as ‘what does this data mean over the longer term?’ and ‘what construction of the body is implied by these kinds of tools?’ (Almost always it is a ‘healthy normal body’).
Personal informatics systems and devices allow for tracking of aspects of life like diet and exercise and we live in a society where individual lifestyles and behaviour are constantly emphasised as a risk factor for illness. So it is perhaps not at all surprising that some people with LTCs have adopted these technologies for self management.
In a recent review of HCI literature Nunes et al [32] outline five categories of how technology can assist with ‘self care’ (‘self care’ is a broader area than self management and covers behaviour like treating minor ailments as outlined by the BMA [3]). Nunes et al review 29 different HCI papers covering conditions such as asthma, fibromyalgia and diabetes and how various different technologies, including personal informatics, were used as self care tools by people with these conditions or their carers.
The category of most relevance to personal informatics is ‘fostering reflection by making contextual information available’ (pp.33:17 [32]). An example would be providing patients with Type 2 diabetes with a smartphone app that tracks activities and food intake [30].
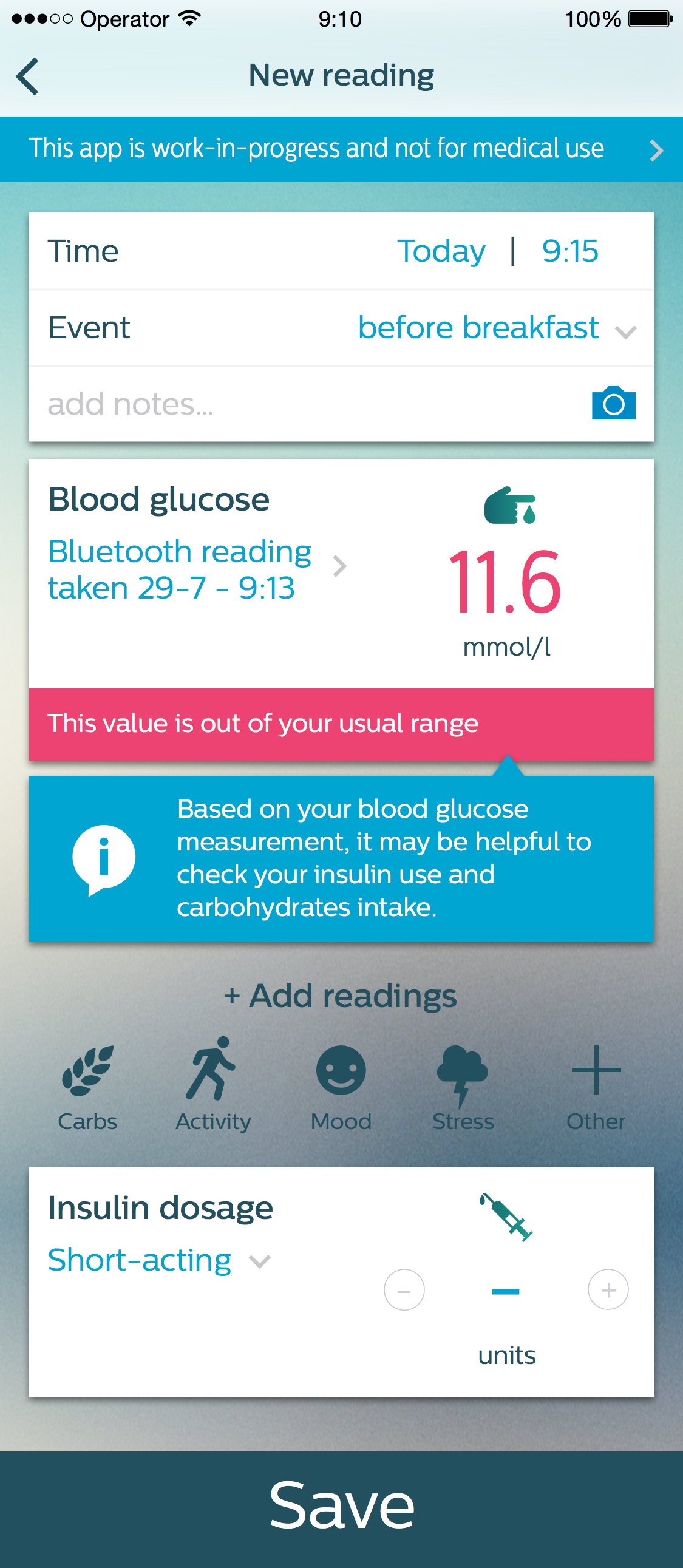
What these type of apps share is an underlying assumption that increased knowledge will give the user power to improve their life: as Nunes et al state “knowing one’s body is essential to achieve control of a chronic condition” (pp.33:17 [32]).
I think the reason I feel uncomfortable with this kind of statement is because my personal experience is that developing a chronic condition involves some acceptance of giving-up control. A pain flare-up can perhaps be made less bad by maintaining a healthy lifestyle but it can’t be entirely prevented.
I think there is a danger that much of the HCI literature adopts an uncritical stance towards an individualised notion of the body and health. I feel it could benefit from more engagement with the sociologies of heath, illness and the body where writers have highlighted the extent to which the dominant narrative of healthism influences society’s norms and values (as outlined in Delvin’s blog post). Without this critical stance I think technology will be designed in a way that unthinkingly replicates these values and their concomitant power structures.
Furthermore, Ancker et al suggest that much of the ‘quantified self’ rhetoric has assumed that people will have an almost unlimited enthusiasm for tracking their bodies. But people with multiple conditions may not want to be constantly reminded that they are ill by having to track all the time [1].
In my blog post on PI I was particularly interested in how it could be used to self manage chronic pain. As Park & Chen remark [33] most of the interest in chronic illness management from HCI and CSCW has focused on “well-known chronic diseases such cancer and diabetes where the impacts and symptoms of the disease are constantly present”.
Issues like chronic pain present particular social problems for sufferers because the symptoms are intermittent and they are not visible [38]. Those with invisible illnesses may therefore find that they need to prove their entitlement to certain types of help or ‘privileges’ of the sick role.
I was fascinated by the comments made by users of a PIS designed to facilitate pain self management and functioning which I found in this paper [11]. Participants wanted the PIS to provide “physical evidence of pain”. They even spoke of wanting a “transparent body that could be read and understood by themselves and others to foster acceptance and overcome stigma”. The participants were wanting the technology to change how their health care professionals understood their pain but in other work Ancker et al found that healthcare professionals trust lab reports far more than the results of self-tracking [1]. For me this highlights what Lupton calls “the valorisation of data” [20] and I see parallels with the argument made by Toyama; that “technology cannot substitute for missing institutional capacity or human intent” (pp.78) [37].

I would argue that these concerns with making the invisible visible are, in part, the result of social, political and cultural pressures to be healthy, productive and working. People unable to fulfil these societal demands and functions are required to prove that they are not shirking and are thus entitled to the ‘sick role’. The participants in the chronic pain study were therefore hoping that the data provided by the PIS could aid social acceptance. However, my critical position is that data and PIS alone can never do this and we should always be wary of demanding too much objectivity from our socially produced and socially understood data.
Online communities
In our session on online communities we learned that for many years researchers have analysed and theorised the reasons why people use social networks like Facebook and Twitter. As Jen commented in her blog post, in 2015 it seems obvious that people use Facebook to ‘look at’, ‘look up’ and ‘keep in touch’ with people but when Joinson [16] wrote his 2008 paper most studies of Facebook had been confined to campus studies of student usage. Jen also found more recent evidence that Facebook improved social ties between friends [5]. There have also been studies of the life-cycle of online communities in general and Stuart’s blog post summarised one of the best-known papers in this area [15].
In terms of use of online communities for self management of long term conditions there has been longstanding interest from the HCI community. Early studies found that online health communities provided members with the chance to connect with others with similar experiences [10] [24]. One of the most well-known of these online health communities is Patients Like Me where the home page exhorts the visitor to “learn from others”, “connect with people like you” and “track your health”.

All of these activities require a certain amount of ‘work’ on behalf of the user. Newman et al [31] interviewed people struggling with weight loss and diabetes management who were using social networking sites for emotional support, motivation, accountability and advice (alongside other online and offline sources). They found that participants put a great deal of effort into thinking about what health information to share and with whom. That is not to say that the effort was not worth it but it does raise the question of how these new forms of technology create new burdens or costs for users as well as benefits.
In terms of the other drawbacks of these communities I would also question the common characterisation of online health communities as non-judgemental or ‘safe’ spaces where peer support is straightforward [14]. I have witnessed many instances of conflict between members of these communities, particularly around the issue of demonstrating ‘wellness’. For example, when a high profile member of one of the Facebook condition groups I belong to did a marathon she was criticised by other members who thought this would add to society’s belittling of the problems associated with that condition. In addition, work by Mankoff et al suggests that the variety and volume of viewpoints can be confusing for those with chronic conditions seeking support online [25].
How does this relate to digital civics? New models of social and health services and ‘The Digital Citizen’
There are significant implications for the digital civics agenda from the increasing use of technology in the area of self management of LTCs. I see this as pivoting around two domains. Firstly, new models of social and health services and secondly, the implied rights and responsibilities of the digital citizen.
All service design involves modelling human behaviour and how people interact with that service, whether these models are made explicit or are implied. If people with long term conditions are using technology to help self manage their condition then health care professionals will need to develop policies and practices for reacting to that. Already we are seeing increasing numbers of hospitals engaging with patients via social media [29]. Yet on an individual level health care professionals can be wary of endorsing online support [13].
New forms of health and social care services are being developed which emphasise ‘patient-power’, ‘co-production’ and ‘peer-support’ [35,36]. Often these services are being designed around perceptions of technology use.
There is also the potential for the huge amounts of health data being shared online to be used for public health purposes. This type of ‘societal computing’ [28] sees the social interactions that are being mediated by online networks like Twitter as a kind of ‘social sensor’. Social media analytics for a social purpose involves collecting and analysing social media data to reveal societal patterns, including health patterns [6, 7, 8].
Running through all of these issues of how health and social services should be configured in the digital age is the question of digital citizenship. Who is the digital citizen and what are her or his rights and responsibilities in relation to health?

Lupton has posited that increasingly services are designed around a neoliberal conception of the “idealised health citizen” who “takes responsibility for her or his health status, wellbeing and productivity without requiring the assistance of the state” [21,23]
Future research?
There is great potential for future research in this area. These are some of the issues I would like to explore myself or read more about:
- Technology-use to self manage invisible illnesses and multi-morbidity: much existing HCI work in the area of chronic illness concentrates on specific conditions which have clear diagnostic markers, like cancer and diabetes, rather than fluctuating or invisible long term conditions (Nunes et al comment on how diabetes has been especially heavily represented in the HCI lit and explain why this might be [32]).
- What are the costs of sharing this type of personal information online? Can we design systems that allow for modification or retraction at a later date? How can people have more ownership and control over what they share? What ‘labour’ is involved in quantifying the body and being a digital health citizen? [26, 27].
- How can health and social care professionals adapt their practice to reflect changed patient behaviour?
- Can health and social services harvest people’s collected informatics and/or shared stories online and what are the technical, ethical and policy implications of this?
- Longitudinal studies would make sense as these are long term conditions. Much of the existing literature reports small-scale studies of bespoke apps focussed on managing a few aspects of a particular condition. I am not sure how sustainable some of these technologies are and I think a ‘lived informatics’ approach [34] requires considering the complexities of living with and tracking chronic conditions over longer time periods. I think this is particularly pertinent in the light of recent work demonstrating health-tracking technology abandonment [9].
- Following the ‘life-cycle’ type analysis of online communities [15] I also think it would be interesting to explore how relationships built around illness develop when members demonstrate ‘wellness’ or improved health.
- What is the social side of personal informatics? I am particularly interested in whether data collected personally can be used to understand societal patterns and support collective action to bring about social change [28]. For example, looking at the environmental, social or economic influences on health rather than just individual behaviour.
In conclusion
These are two huge areas of HCI and I feel I have only scratched the surface of how they relate to digital civics and the self management of long term conditions.
I think there are two central themes that intersect the use of personal informatics and online communities as tools for self management. The first is that of making the invisible visible: at the individual level of ‘demonstrating illness’ via personal informatics and at the societal level whereby people can gain greater visibility for their condition as a group than they could as an individual with a long term condition*.
The second is making connections. At the individual level this means between circumstances/behaviour and symptoms (knowledge which can potentially be gained from tracking or from feedback when sharing experiences). At the societal level this means making connections with others who share one’s condition and can therefore offer support and perhaps even begin to act collectively.
I have personally found great help from technology in managing my long term conditions. Making connections with others who have similar experiences and using PIS to track triggers and to motivate myself to follow diet and exercise advice has definitely improved my life.
However, what I think is problematic is that there has not been enough reflection in HCI on the social norms and pressures which shape how we use technology for self management and what we want that technology to do. I think it is vital to reflect on these social aspects because if we don’t we can design technology that unthinkingly reproduces existing power structures and places too much emphasis on individual lifestyle rather than the social determinants of health. I am also keen to explore how or if data can ever change power relationships in the ways required for the digital civics agenda to be fully realised.
** There is a flipside to this theme: in my blog post on Crowd Work I read a paper arguing for the value of online crowd work for disabled people who do not want their disabled status to be known in the work context
REFERENCES
- Jessica S Ancker, Holly O Witteman, Baria Hafeez, Thierry Provencher, Mary Van de Graaf, and Esther Wei. 2015. “You Get Reminded You’re a Sick Person”: Personal Data Tracking and Patients With Multiple Chronic Conditions. Journal of medical Internet research 17, 8: e202. http://doi.org/10.2196/jmir.4209
- Kate Barker. 2014. A new settlement for health and social care, Interim report. The King’s Fund: 86. http://www.kingsfund.org.uk/publications/new-settlement-health-and-social-care
- BMA. 2015. Self care : question & answer. British Medical Association. Retrieved fromhttp://www.bma.org.uk/working-for-change/improving-and-protecting-health/self-care
- Susanne Bødker. 2006. When second wave HCI meets third wave challenges. 4th Nordic Conference on Human-Computer Interaction …, October: 14–18. http://doi.org/10.1145/1182475.1182476
- Moira Burke and Robert E. Kraut. 2014. Growing closer on facebook. Proceedings of the 32nd annual ACM conference on Human factors in computing systems – CHI ’14, 4187–4196. http://doi.org/10.1145/2556288.2557094
- Munmun De Choudhury, Scott Counts, and Eric Horvitz. 2013. Social media as a measurement tool of depression in populations. Proceedings of the 5th Annual ACM Web Science Conference on – WebSci ’13: 47–56. http://doi.org/10.1145/2464464.2464480
- Munmun De Choudhury. Anorexia on Tumblr: A Characterization Study. http://doi.org/10.1145/2750511.2750515
- Munmun De Choudhury. Role of Social Media in Tackling Challenges in Mental Health. http://dl.acm.org/citation.cfm?id=2509921
- James Clawson, Jessica A Pater, Andrew D Miller, Elizabeth D Mynatt, and Lena Mamykina. No Longer Wearing: Investigating the Abandonment of Personal Health-Tracking Technologies on Craigslist. http://dl.acm.org/citation.cfm?id=2807554&CFID=573795698&CFTOKEN=51799259
- Shelly Farnham, Lili Cheng, Linda Stone, et al. 2002. HutchWorld : Clinical Study of Computer-Mediated Social Support for Cancer Patients and Their Caregivers. CHI 2002, 1: 375–382. http://doi.org/10.1145/503376.503444
- Sergio Felipe, Aneesha Singh, Caroline Bradley, Amanda Cdec Williams, and Nadia Bianchi-berthouze. 2015. Roles for Personal Informatics in Chronic Pain. 9th International Conference on Pervasive Computing Technologies for Healthcare, IEEE. http://dx.doi.org/10.4108/icst.pervasivehealth.2015.259501
- Christine Gallagher. 2015. Evidence Search and Synthesis NHS Education for Scotland. Retrieved from http://www.widgetlibrary.knowledge.scot.nhs.uk/media/WidgetFiles/1010550/Final – social networking evidence summary_1_.pdf
- K Gordon, H Rice, N Allcock, et al. 2015. Barriers to Self-Management of Chronic Pain in Primary Care. Retrieved from http://painconcern.org.uk/wp-content/uploads/2015/03/Barriers-to-Self-Management-Report-Final.pdf
- Kevin O Hwang, Allison J Ottenbacher, Angela P Green, et al. 2010. Social support in an Internet weight loss community. International journal of medical informatics 79, 1: 5–13. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3060773/
- Alicia Iriberri and Gondy Leroy. 2009. A Life Cycle Perspective on Online Community Success. ACM Computing Surveys 41: 1–29. Retrieved from http://portal.acm.org/citation.cfm?doid=1459352.1459356
- Adam N. Joinson. 2008. “Looking at”, “Looking up” or “Keeping up with” People? Motives and uses of Facebook. Chi 2008: 1027–1036. http://dl.acm.org/citation.cfm?id=1357213
- Ian Li, Anind Dey, and Jodi Forlizzi. A Stage-Based Model of Personal Informatics Systems. http://dl.acm.org/citation.cfm?doid=1753326.1753409&CFID=556045048&CFTOKEN=50563404
- Cristina Lonardi. 2007. The passing dilemma in socially invisible diseases: Narratives on chronic headache. Social Science & Medicine 65: 1619–1629. http://doi.org/10.1016/j.socscimed.2007.07.007
- Deborah Lupton. You are Your Data: Self-tracking Practices and Concepts of Data. Forthcoming book chapter. Retrieved from http://ssrn.com/abstract=2534211
- Deborah Lupton. Self-tracking Cultures: Towards a Sociology of Personal Informatics. http://doi.org/10.1145/2686612.2686623
- Deborah Lupton. “Mastering Your Fertility”: The Digitised Reproductive Citizen. In Negotiating Digital Citizenship: Control, Contest and Culture, Anthony Mccosker, Sonja Vivienne and Amelia Johns (eds.). Rowman & Littlefield, London. Retrieved from http://papers.ssrn.com/sol3/papers.cfm?abstract_id=2679402
- Deborah Lupton. 2013. Quantifying the body: monitoring and measuring health in the age of mHealth technologies. Critical Public Health 23, 4: 393–403. http://doi.org/10.1080/09581596.2013.794931
- Deborah Lupton. 2013. The digitally engaged patient: Self-monitoring and self-care in the digital health era. Social Theory & Health 11: 256–270. http://doi.org/10.1057/sth.2013.10
- Diane Maloney-Krichmar and Jenny Preece. 2005. A multilevel analysis of sociability, usability, and community dynamics in an online health community. ACM Transactions on Computer-Human Interaction 12, 2: 201–232. http://doi.org/10.1145/1067860.1067864
- Jennifer Mankoff, Kateryna Kuksenok, Jennifer Rode, Sara Kiesler, and Kelly Waldman. 2011. Competing Online Viewpoints and Models of Chronic Illness. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ’11): 589–598. http://doi.org/DOI=http://dx.doi.org/10.1145/1978942.1979027
- Anthony Mccosker and Raya Darcy. 2013. LIVING WITH CANCER: Affective Labour, Self-Expression and the Utility of Blogs. Information, Communication & Society 16, 8: http://www.tandfonline.com/doi/abs/10.1080/1369118X.2012.758303
- Anthony Mccosker. Negotiating illness bloggers’ expressive worlds: adapting digital ethnography Background: research context, problem and aims. (work in progress).
- Andrés Monroy-Hernández, Shelly Farnham, Emre Kiciman, Scott Counts, and Munmun De Choudhury. 2013. Smart Societies: From Citizens as Sensors to Collective Action. Interactions July & August 2013. http://dl.acm.org/citation.cfm?id=2486249&CFID=556045048&CFTOKEN=50563404
- S Anne Moorhead, Diane E Hazlett, Laura Harrison, Jennifer K Carroll, Anthea Irwin, and Ciska Hoving. 2013. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. Journal of medical Internet research 15, 4: e85. http://doi.org/10.2196/jmir.1933
- Raviraja Nachman, Lama and Baxi, Amit and Bhattacharya, Sangeeta and Darera, Vivek and Deshpande, Piyush and Kodalapura, Nagaraju and Mageshkumar, Vincent and Rath, Satish and Shahabdeen, Junaith and Acharya. 2010. Jog Falls: A Pervasive Healthcare Platform for Diabetes Management. Pervasive Computing 6030: 94–111. http://doi.org/10.1007/978-3-642-12654-3_6
- Mark W. Newman, Debra Lauterbach, Sean A. Munson, Paul Resnick, and Margaret E. Morris. 2011. It’s not that i don’t have problems, i’m just not putting them on facebook. Proceedings of the ACM 2011 conference on Computer supported cooperative work – CSCW ’11, 341. http://doi.org/10.1145/1958824.1958876
- Francisco Nunes, Nervo Verdezoto, Geraldine Fitzpatrick, Morten Kyng, Erik Grönvall, and Cristiano Storni. 2015. 33 Self-Care Technologies in HCI: Trends, Tensions, and Opportunities. ACM Trans. Comput.-Hum. Inter-act. Article 22, 33. http://doi.org/10.1145/2803173
- Sun Young Park and Yunan Chen. 2015. Individual and Social Recognition : Challenges and Opportunities in Migraine Management. 1540–1551. http://doi.org/10.1145/2675133.2675248
- John Rooksby, Mattias Rost, Alistair Morrison, and Matthew Chalmers. Personal Tracking as Lived Informatics. http://doi.org/10.1145/2556288.2557039
- Cristiano Storni. 2014. Design challenges for ubiquitous and personal computing in chronic disease care and patient empowerment: A case study rethinking diabetes self-monitoring. Personal and Ubiquitous Computing 18, 5: 1277–1290. http://doi.org/10.1007/s00779-013-0707-6
- Melanie Swan. 2009. Emerging patient-driven health care models: an examination of health social networks, consumer personalized medicine and quantified self-tracking. International journal of environmental research and public health 6, 2: 492–525. http://doi.org/10.3390/ijerph6020492
- Kentaro Toyama. 2011. Technology as amplifier in international development. Proceedings of the 2011 iConference on – iConference ’11: 75–82. http://doi.org/10.1145/1940761.1940772
- Margaret Vickers. 1997. Life at work with “invisible” chronic illness (ICI): the “unseen”, unspoken, unrecognized dilemma of disclosure. Journal of Workplace Learning Management Review Journal of International Education in Business Iss Journal of Workplace Learning 9, 10: 240 – 252. Retrieved from http://dx.doi.org/10.1108/13665629710190040
- http://selfmanagementuk.org/what-self-management. Retrieved from http://selfmanagementuk.org/what-self-management
Leave a Reply Cancel reply
You must be logged in to post a comment.